Bienvenue au
Cabinet Dentaire Davarpanah
Implantologie | Chirurgie | Dentisterie esthétique
Notre équipe pluridisciplinaire a pour ambition de vous proposer une prise en charge d’excellence dans les domaines suivants : implants dentaires, chirurgie buccale (extractions dentaires), greffes osseuses, parodontologie (soins des gencives et détartrage), greffes esthétiques de gencive, soins prothétiques et restaurations esthétiques.
L’association synergique de nos différentes spécialités permet d’améliorer la prise de décision thérapeutique et la mise en œuvre des différentes étapes de traitement.


Notre équipe
Les praticiens
Les assistantes

Vida

Aurélie

Shorena

Maegan

Vanessa

Sabrina

Viktorya

Sabrina

Claire

Alexandra

Linh Chi

Linh

Mary
Nos orientations thérapeutiques
Spécialités du cabinet
Notre expertise rassemble l’implantologie, la chirurgie orale (extractions et greffes osseuses), la parodontologie et les greffes esthétiques de gencive ainsi que les soins restaurateurs et prothétiques.
Nous travaillons en étroite collaboration avec des orthodontistes et des endodontistes (traitements de dévitalisation des canaux dentaires).
Nos valeurs
Écoute et prise en charge rapide
Prise en charge globale pluridisciplinaire

Réhabilitation Globale
En cas de déficit fonctionnel ou esthétique conséquent, la prise en charge thérapeutique nécessitera l’association synergique de différentes spécialités cliniques (implantologie et prothèse notamment). L’étroite collaboration entre nos différents praticiens ainsi que la planification en amont du traitement seront fondamentales afin d’améliorer le résultat esthétique.

Analyse esthétique et diagnostic pré-prothétique
L’analyse esthétique pré-prothétique est fondamentale et permet d’améliorer la prédictibilité du résultat clinique, notamment lorsque la situation clinique présente une forte composante esthétique.
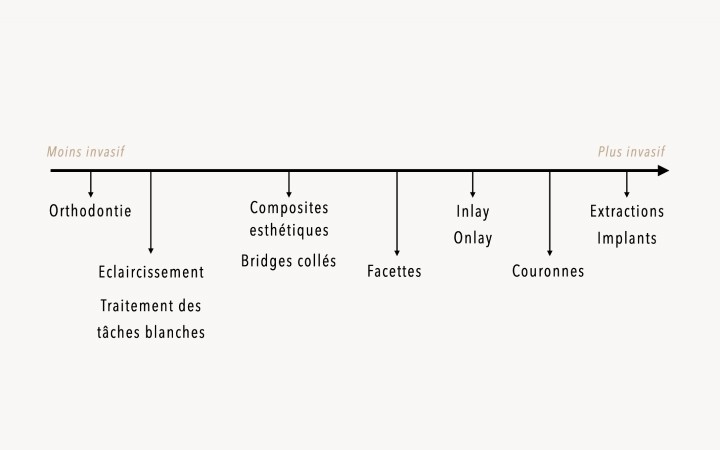
Philosophie du gradient thérapeutique
Toutes nos décisions thérapeutiques sont guidées par un souci de préservation tissulaire maximale.
Urgences
En cas d’urgence esthétique ou douloureuse, nous veillons à ce que la prise en charge du patient se fasse dans les meilleurs délais. Contactez-nous par mail ou par téléphone.
Publications, articles & livres
Notre activité clinique est complémentaire, sous-tendue et appuyée par des connaissances scientifiques.















 Implants dentaires
Implants dentaires 
 Esthétique et prothèse
Esthétique et prothèse 


 Suivi et détartrage
Suivi et détartrage